In this section
Learn:
- Why certified health IT is important to your practice
- How to compare certified health IT products
- How APIs can ease information exchange
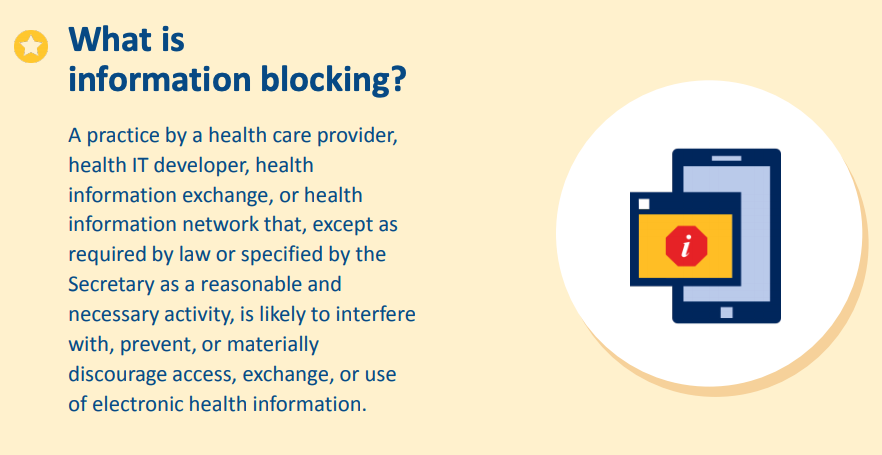
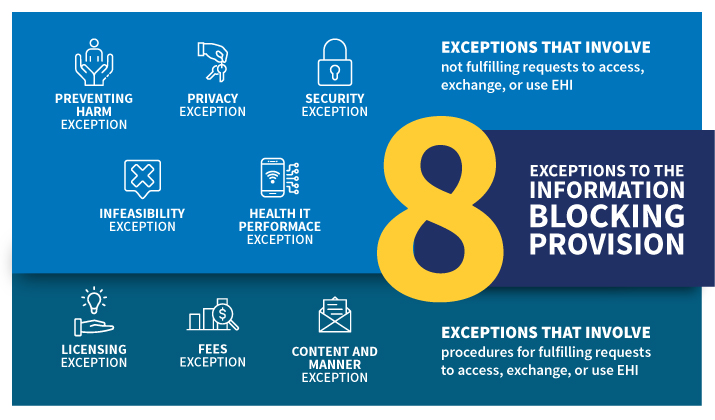
- How to recognize information blocking
- How to report issues with certified health IT products to ONC
How can certified health IT help my practice?
Certified health IT can help your practice by:
- Making electronic prescribing available, which is safer, cheaper, and more convenient for clinicians and patients
- Supporting electronic transitions of care, closing referral loops, and giving clinicians straightforward and secure access to their patients’ records from outside organizations
- Making the process for patients to get their personal health information less time-consuming and tedious for all parties while maintaining confidentiality
- Automating the process of sending data to immunization registries
- Facilitating reporting of electronic clinical quality measures to the Centers for Medicare & Medicaid Services (CMS)
The Office of the National Coordinator for Health Information Technology (ONC) oversees the Health IT Certification Program for health IT modules — including electronic health records (EHR). The certification program sets several nationwide standards including:
- Health IT standards
- Implementation specifications
- Certification criteria
Certified health IT plays a vital role in establishing a nationwide, connected, and interoperable health information infrastructure. Health IT modules certified under the ONC Health IT Certification Program are listed on ONC’s Certified Health IT Product List (CHPL).
How certified health IT benefits your practice
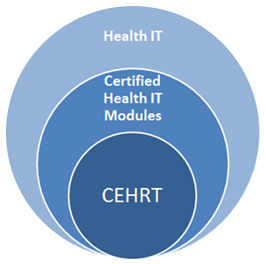
Certain health care payment programs — including the Promoting Interoperability Programs for hospitals and the Merit-based Incentive Payment System (MIPS) under the Quality Payment Program for eligible clinicians (formerly the EHR Incentive or Meaningful Use programs) — require the use of certified health IT. CMS calls the minimum set of required certification functionalities that program participants must use to meet the requirements of these incentive programs Certified EHR Technology (CEHRT).
Using certified health IT — including standards-based application programming interfaces (APIs), electronic exchange of clinical care documents, and other standards-based transactions such as e-prescribing — improves care coordination. Certification provides a baseline assurance that a health IT module will perform clinical care and data exchange functions in accordance with interoperability standards and user-centered design. The benefits of standard data capture and interoperable exchange of information include enhanced patient safety, usability, privacy, and security.
Standards incorporated into the ONC Health IT Certification Program include vocabulary code sets, like SNOMED-CT®, that ensure consistent clinical terminology between systems. Standards for structuring clinical content include the Consolidated Clinical Document Architecture (C-CDA), which is discussed in section 1 of this playbook. The C-CDA allows different EHR systems to send and receive a patient’s clinical care summary while retaining the same meaning across systems. Other standards for exchanging patients’ health information include the Fast Healthcare Interoperability Resources (FHIR®) standard, which enables the APIs.
To date, ONC has issued 3 editions of health IT certification criteria:
- 2011 Edition (retired)
- 2014 Edition (retired)
- 2015 Edition
The 21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program Final Rule (ONC Cures Act Final Rule) made several changes to the existing 2015 Edition Health IT Certification Criteria and adopted new program requirements from the 21st Century Cures Act. Specifically, the ONC Cures Act Final Rule:
- Introduced a small number of new certification criteria
- Revised several existing certification criteria
- Removed several certification criteria
While all of the existing and newly added criteria are part of the 2015 Edition, ONC refers to them collectively as the 2015 Edition Cures Update on the CHPL and in program resources. This helps to distinguish changes to the ONC Health IT Certification Program adopted by the Final Rule.
Each edition builds on the previous version by adopting newer standards and more advanced health IT functions. The goal: continually move toward nationwide interoperability, improved clinical care, and better health information exchange.
Many programs and organizations encourage or require the use of health IT certified under the ONC Health IT Certification Program — in addition to the Promoting Interoperability Programs. Check out this list of programs that reference the certification program.