New Data Show Nearly One-Third of Hospitals Can Access PDMP Data within their EHR
Elisabeth Myers and Talisha Searcy | October 23, 2019
Combatting the opioid crisis is a top priority for the U.S. Department of Health and Human Services (HHS) and the nation. Equipping healthcare providers with easy access to data about their patients’ opioid prescriptions is one strategy to help reduce opioid misuse. Prescription Drug Monitoring Programs (PDMPs) are state-run databases that collect patient-specific prescription information at the point of care, or when a controlled substance is dispensed. PDMPs can be a tool for health care providers to improve prescribing practices, target treatment efforts to at risk patients, and mitigate the risk of potential abuse or fraud by patients who obtain prescriptions from multiple providers.
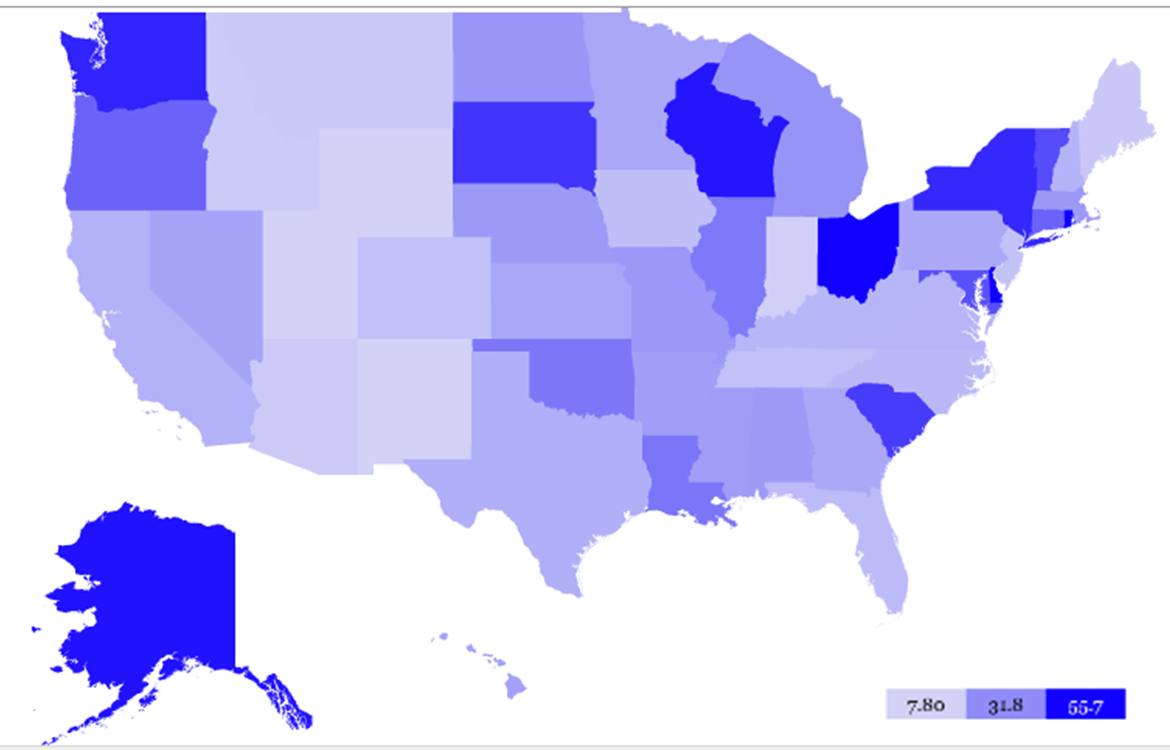
Since 2011, the Office of the National Coordinator for Health Information Technology (ONC) has worked with stakeholders and federal partners to integrate health information technology (IT) tools and PDMP access and query functionality into clinical workflows. Workflow integration may involve the ability for clinicians to access and query the state PDMP within a hospital’s electronic health record (EHR) system. Access and query functions within the EHR may help the clinician by facilitating access to PDMP information to support clinical decision-making at the point of care. ONC’s new analysis of 2017 data from the American Hospital Association Annual Survey IT Supplement shows that nearly one in three hospitals access their state’s PDMP using their hospital’s EHR. This data provides the first evidence of how hospitals are accessing PDMP data.
Health IT integration and enhanced user interfaces can be effective in addressing barriers to using PDMPs. This was demonstrated by earlier HHS studies. The use of content and vocabulary standards and standards-based health information exchange may also facilitate the integration of PDMP data into a longitudinal care record.
ONC continues to execute a multi-pronged approach to advance the use of health IT to address the nation’s opioid epidemic. For instance, as part of HHS-wide efforts to implement the provisions of the Support Act, ONC is collaborating with federal partners to support standards-based approaches to further PDMP access and query functionality within EHRs, as well as data exchange and integration within health IT systems. ONC is also analyzing and identifying opioid use disorder (OUD) related and PDMP specific data elements as represented using content and vocabulary standards, mapping PDMP data elements with Fast Healthcare Interoperability Resources (FHIR) to support standards-based application programming (API) solutions for PDMP data exchange, and developing electronic specifications for clinical decision support artifacts related to clinical best practice guidelines for PDMP queries. Lastly, ONC has an upcoming review of state health IT policy and technical landscapes designed to address the opioid epidemic. All of these efforts are important for streamlining clinicians’ access to PDMP data.
PDMP data enables clinicians to make informed decisions and take appropriate action before prescribing an opioid. By giving providers information about a patient’s medical history and prescription drug use, PDMPs can improve prescribing practices. We look forward to continuing to work with stakeholders to identify ways to enhance clinicians’ access to PDMP data; which is an important tool to combatting the opioid crisis.
Figure 1. Percent of U.S. non-federal acute care hospitals that can access their state’s PDMPs within their Hospital’s EHR by State, 2017
Source: ONC’s analysis of 2017 AHA Annual Survey Information Technology Supplement Data