
An official website of the United States government
Here’s how you know
Official websites use .gov
A
.gov
website belongs to an official government organization in the
United States.
Secure .gov websites use HTTPS
A
lock
(
) or
https://
means you’ve safely connected to the .gov website. Share sensitive
information only on official, secure websites.
Electronic Prescribing of Controlled Substances Among Office-Based Physicians, 2017-2019
No. 58 | June 2022
Electronic prescribing of controlled substances (EPCS) technology enables clinicians to securely transmit prescriptions for controlled substances to a pharmacy (1). In 2018, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT Act) mandated the prescribing of Schedule II, III, IV, or V controlled substances under Medicare Part D to be done using EPCS technology starting January 1, 2021 (2). This mandate was implemented and finalized through the Centers for Medicare & Medicaid Services (CMS) Calendar Year (CY) 2021 Physician Fee Schedule specifying appropriate exceptions and providing compliance flexibilities through January 1, 2022 (3). This brief provides national estimates of physicians’ use of EPCS technology in 2019 from the National Electronic Health Record Survey. These findings serve as basedline estimates upon which to examine the future impact of the Part D EPCS mandate going into effect. The brief also explores variation in the use of EPCS by physician characteristics; including practice size and ownership, physician specialty, geographic location, and frequency of a physician prescribing controlled substances.
Highlights
- Among physicians that prescribe controlled substances, the proportion that use EPCS increased by 12 percentage points between 2017 and 2019.
- Physicians that prescribe controlled substances more frequently use EPCS at higher rates compared to physicians that prescribe controlled substances less frequently.
- Solo practitioners and providers in physician-owned practices used EPCS at lower rates compared to practices with multiple physicians and those owned by corporations or hospitals.
- The proportion of physicians in community health centers using EPCS increased from 26 percent to 61 percent between 2017 and 2019.
The percentage of physician prescribers of controlled substances that used EPCS technology increased between 2017 and 2019.
Findings
- The proportion of physicians that reported prescribing controlled substances did not increase between 2017 and 2019.
- Among physicians that prescribe controlled substances, the proportion that use EPCS increased by 12 percentage points between 2017 and 2019.
- In 2019, nine in 10 physicians reported prescribing controlled substances, and among these physicians four in 10 used EPCS technology.
Figure 1: Percent of office-based physicians that prescribe controlled substances and use EPCS technology, 2017-2019.

Note: *Statistically significant from 2017 (p<0.05).
Nearly half of physicians used electronic methods to prescribe non-controlled medications, but relied on paper to prescribe controlled substances in 2019.
Findings
- Nine in 10 physicians used electronic methods to prescribe non-controlled medications in 2019.
- The proportion of physicians who used electronic methods to prescribe non-controlled medications, but relied on paper to prescribe controlled substances decreased by 10 percentage points from 2017 to 2019 (See Appendix Table A2).
- One in 10 physicians used paper to prescribe both controlled and non-controlled substances in 2019.
Table 1: Percent of office-based physicians that use paper and electronic methods to prescribe controlled and non-controlled substances, 2019.
| Method to Prescribe Controlled Substances | |||
|---|---|---|---|
| Electronic | Paper | ||
| Method to Prescribe Non-Controlled Substances Substances | Electronic | 43% | 47% |
| Paper | 1% | 9% | |
Note: Denominator is among those who prescribe controlled substances.
Physicians that prescribe controlled substances more frequently use EPCS at higher rates compared to physicians that prescribe controlled substances less frequently.
Findings
- Among physicians that report “often” prescribing controlled substances, six in 10 reported using EPCS in 2019.
- Among physicians that report “sometimes” prescribing controlled substances, about half reported using EPCS in 2019.
- Among physicians that report “rarely” prescribing controlled substances, about a quarter reported using EPCS in 2019.
Figure 2: Percent of office-based physicians that use EPCS technology by frequency of prescribing controlled substances, 2019.
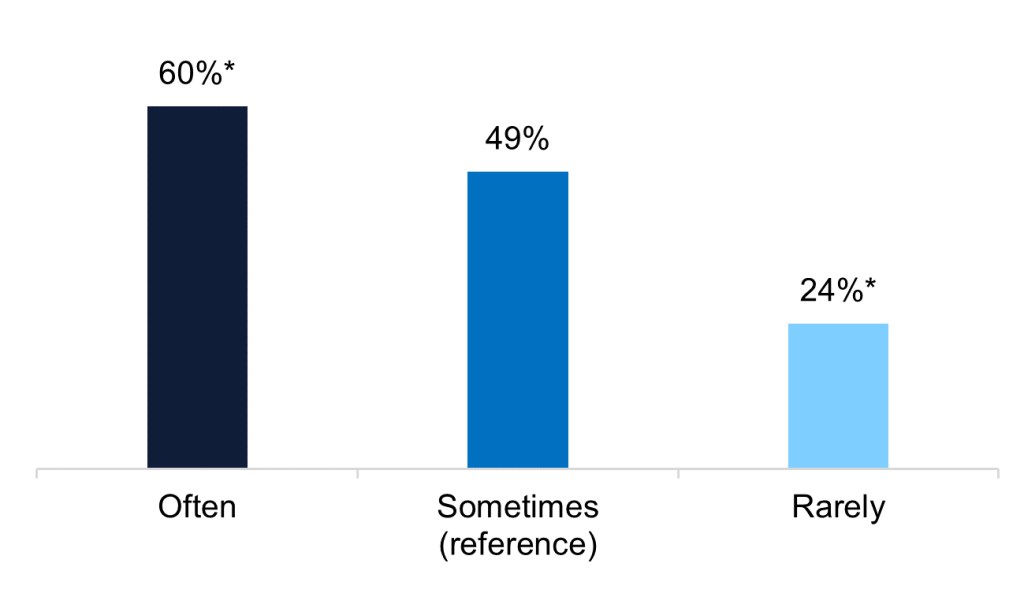
Notes: *Statistically significant from “Sometimes” reference group (p<0.05). 29% of physicians reported that they “Often” prescribe controlled substances, 31% of physicians report that they “Sometimes” prescribe controlled substances, and 31% of physicians reported that they “Rarely” prescribe controlled substances.
Solo practitioners used EPCS at lower rates compared to practices with multiple physicians.
Findings
- About three in 10 solo practitioners used EPCS in 2019 compared to about half of physicians who worked in practices with 11 or more physicians.
- About six in 10 physicians in practices owned by hospital, corporation, community health center used EPCS in 2019 – these physicians used EPCS at higher rates compared to practices owned by a physician or physician group.
- Physicians in a single specialty group used EPCS at lower rates compared to physicians in a multispecialty group (42% vs. 50%).
- Physicians that treated Medicare and Medicaid patients used EPCS at similar rates to the national average.
- About four in 10 physicians used EPCS in both rural and urban areas.
Table 2: Percent of office-based physicians that use EPCS technology by practice characteristics, 2019.
| Practice Characteristics | Use EPCS Technology (Among those who Prescribe Controlled Substances) |
|---|---|
| Practice Size | |
| 1 physician (reference) | 30% |
| 2-5 physicians | 49%* |
| 6-10 physicians | 46%* |
| 11 or more physicians | 52%* |
| Practice Ownership | |
| Physician/Physician Group (reference) | 36% |
| Insurance Company or Corporation | 59%* |
| Community Health Center | 61%* |
| Hospital | 58%* |
| Specialty Group | |
| Single Specialty (reference) | 42% |
| Multispecialty | 50%* |
| Medicare Physicians | |
| Treat Medicare Patients | 43% |
| Do Not Treat Medicare Patients | 48% |
| Medicaid Physicians | |
| Treat Medicaid Patients | 44% |
| Do Not Treat Medicaid Patients | 41% |
| Geographic Location | |
| Rural (reference) | 43% |
| Urban | 44% |
Notes: *Statistically significant from reference group (p<0.05)
The proportion of physicians using EPCS in community health centers more than doubled between 2017 and 2019.
Findings
- The proportion of physicians in community health centers using EPCS increased from 26 percent to 61 percent between 2017 and 2019.
- The proportion of physicians in physician-owned practices using EPCS increased from 25 percent to 36 percent between 2017 and 2019.
- The proportion of physicians in hospital-owned practices using EPCS increased from 44 percent to 58 percent between 2017 and 2019.
Figure 3: Percent of office-based physicians that use EPCS technology by practice ownership, 2017-2019.

Notes: *Statistically significant from 2017 (p<0.05)
Physicians practicing in areas where there is a greater shortage of mental health professionals report using EPCS at lower rates compared to areas where there is less of a shortage.
Findings
- About three in 10 physicians practicing in areas where the whole county is designated as a mental health professional shortage area used EPCS in 2019.
- About half of physicians practicing in areas where there is no mental health professional shortage area or where only part of the county is designated as a shortage area report using EPCS.
Figure 4: Percent of office-based physicians that use EPCS technology by mental health care provider shortage area, 2019.

Note: *Statistically significant from reference group (p<0.05)
Usage of EPCS technology nearly doubled among psychiatrists and neurologists between 2017 and 2019.
Findings
- About half of primary care physicians used EPCS in 2019 – a 19 percentage point increase from 2017.
- About four in 10 surgical and medical specialty physicians used EPCS in 2019.
- About two thirds of psychiatrists and neurologists used EPCS in 2019.
- The proportion of psychiatrists and neurologists using EPCS increased by more than 30 percentage points between 2017 and 2019.
Table 3: Percent of office-based physicians that use EPCS technology by physician specialty, 2017-2019.
| Specialty |
Use EPCS Technology (Among specialties that frequently prescribe controlled substances ^) | |
|---|---|---|
| 2017 | 2019 | |
| All Physicians | 32% | 44%* |
| Primary Care | 32% | 51%* |
| Internal Medicine | 28% | 52%* |
| General or Family Practice | 34% | 47%* |
| Pediatrics | 34% | 59%* |
| Medical Specialty | 31% | 38% |
| Psychiatry | 36% | 68%* |
| Neurology | 30% | 66%* |
| Obstetrics & Gynecology | 32% | 46% |
| Surgical Specialty | 31% | 35% |
Note: *Statistically significant from 2017 (p<0.05). ^These categories represent specialties where more than 85% of physicians reported prescribing controlled substances in 2019. Due to small sample sizes, we were unable to report estimates for additional specialties.
Summary
The percentage of physician prescribers of controlled substances that used EPCS technology increased between 2017 and 2019, from 32 to 44 percent. Most physicians—90%—prescribe controlled substances so the use of EPCS technology has room to grow. Increasing the use of EPCS is significant because similar to e-prescribing, EPCS has the potential to reduce provider burden and improve care coordination by preventing data entry errors, avoiding pharmacy calls to prescribers to clarify written instructions, and eliminating the need to coordinate and manage paper prescriptions between doctors, patients, pharmacies, and other care sites. These tools can also improve patient safety by alerting prescribers of potential drug interactions, inappropriate doses, allergies, and underlying patient conditions (1).
The rates of EPCS are lower than e-prescribing because the requirements to set up EPCS are more stringent. These requirements, estabilshed by the Drug Enforcement Agency, include identity proofing to verify a provider is authorized to prescribe controlled substances, two-factor authentication for health care providers who sign an EPCS prescription, as well as detailed recordkeeping requirements to assist with identifying auditable events and security breaches (4). It is likely partly due to these increased requirements, that among physicians who prescribe controlled substances, nearly half of these providers still relied on paper when prescribing controlled substances. Encouragingly, frequent prescribers of controlled substances reported using EPCS at higher rates compared to those who rarely prescribed controlled substances (60% vs. 24%). Nearly all psychiatrists and neurologists reported prescribing controlled substances. These specialties had the highest rates of reported EPCS use and also had large increases between 2017 and 2019. This likely reflects the value proposition for meeting the requirements for EPCS are higher for frequent prescribers of controlled substances.
This brief also identifies significant variation in use of EPCS by practice size and ownership. These findings indicate that costs and lack of financial support may be barriers to implementing EPCS technology for physicians with fewer resources (5). For example, only 30 percent of solo practitioners and 36 percent of providers in physician-owned practices reported using EPCS. These rates were lower compared to practices with 11 or more physicians (52%) and among practices owned by a corporation (59%) or hospital (58%). Similarly, physicians practicing in mental health provider shortage areas also reported using EPCS at lower rates compared to physicians practicing in non-shortage areas (31% vs. 50%). This indicates that areas of the country with fewer mental health providers, such as psychiatrists, may be lagging behind with use of EPCS. This is significant because an estimated 149 million Americans (45% of the US population) live in a mental health provider shortage area (7). In contrast, physicians working in community health centers or federally qualified health centers (FQHC)’s rates of engaging in EPCS was relatively high, doubling between 2017 and 2019 (increase from 26% to 61%). Previous research has shown that FQHCs are playing an increasing role in providing substance use disorder counseling and treatment services (6). The Health Resources & Services Administration has also funded organizations to provide training and technical assistance to support the adoption and advancement of health IT among FQHCs (8). This may explain the growth in EPCS use in comparison to other types of practices with fewer resources.
The results from this analysis show an increase in the use of EPCS between 2017 and 2019 in various physician practices bringing them closer to compliance of the federal mandate. This is consistent with more recent findings from Surescripts, which includes both hospital-based prescribers in addition to office-based prescribers (9). However, our analysis of 2019 office-based physician survey data suggests that works remains for all Part D providers to achieve full compliance under the SUPPORT Act, particularly practices with fewer resources and those serving vulnerable populations. The Office of the National Coordinator for Health IT has published the Health IT Playbook, which is a resource for health care providers and other stakeholders to use to optimize the safety and use of their electronic health records. The Playbook also includes educational materials for health care providers about the benefits of EPCS to support the appropriate prescribing of opioids and other controlled substances.
Data Source and Methods
The Centers for Disease Control and Prevention’s National Center for Health Statistics conducts the National Electronic Health Records Survey (NEHRS) survey on an annual basis. Physicians included in this survey provide direct patient care in office-based practices and community health centers; excluded are those who do not provide direct patient care (radiologists, anesthesiologists, and pathologists). Additional documentation regarding the survey is here: https://www.cdc.gov/nchs/nehrs/index.html
References
- Office of the National Coordinator for Health IT. Health IT Playbook. Section 4. Opioid Epidemic & Health IT. https://www.healthit.gov/playbook/opioid-epidemic-and-health-it/
- Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act, Section 2003. https://www.congress.gov/bill/115th-congress/house-bill/6/text
- Centers for Medicare & Medicaid Services. CY 2022 Payment Policies under the Physician Fee Schedule and other Changes to Part B Payment Policies. https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf
- Drug Enforcement Agency. Interim Final Rule. Electronic Prescribing of Controlled Substances. https://www.govinfo.gov/content/pkg/FR-2010-03-31/pdf/2010-6687.pdf
- Achar S., Sinha N., & Norcross W. (July 2021). The Adoption and Increased Use of Electronic Prescribing of Controlled Substances. Journal of Medical Regulation. 107(2): 8-16.
- Zur J., Tolbert J., Sharac J., & Markus A. (July 2018). The Role of Community Health Centers in Addressing the Opioid Epidemic. Kaiser Family Foundation Issue Brief. Available Here: https://files.kff.org/attachment/Issue-Brief-The-Role-of-Community-Health-Centers-in-Addressing-the-Opioid-Epidemic
- National Institute for Health Care Management. (May 2022). Prioritizing Mental Health Care In America. Available here: https://nihcm.org/publications/prioritizing-mental-health-care-in-america?utm_source=NIHCM+Foundation&utm_campaign=d8ec96efd0-Prioritizing_Mental_Health_Infographic&utm_medium=email&utm_term=0_6f88de9846-d8ec96efd0-167772052
- Health Resources & Services Administration. Bureau of Primary Health Care Health Center Program. Health Center Controlled Networks Notice of Funding Opportunity (FY 2019). Available Here: https://bphc.hrsa.gov/programopportunities/fundingopportunities/HCCN/hrsa-19-011-nofo.pdf
- Surescripts. 2021 National Progress Report. Available here: https://surescripts.com/docs/default-source/national-progress-reports/2021-national-progress-report.pdf?sfvrsn=71fcbe15_12
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of Technical Strategy and Analysis, and Vaishali Patel, the Data Analysis Branch Chief.
Suggested Citation
Johnson C. & Estrada M. (June 2022). Electronic Prescribing of Controlled Substances Among Office-Based Physicians, 2017-2019. ONC Data Brief, no.58. Office of the National Coordinator for Health Information Technology: Washington DC.
Appendix
Appendix Table A1: Survey questions assessing hospital capabilities to enable patient electronic access to health information
| Question Text | Response Options |
|---|---|
| How frequently do you prescribe controlled substances? |
|
| How frequently are prescriptions for controlled substances sent electronically to the pharmacy? |
|
Appendix Table A2: Percent of office-based physicians that use paper and electronic methods to prescribe controlled and non-controlled substances, 2017.
| Method to Prescribe Controlled Substances | |||
|---|---|---|---|
| Electronic | Paper | ||
| Method to Prescribe Non-Controlled Substances | Electronic | 32% | 57% |
| Paper | <1% | 11% | |
Note: Denominator is among those who prescribe controlled substances.
