According to a recent American Hospital Association (AHA) survey, most hospitals know about the Trusted Exchange Framework and Common AgreementSM (TEFCASM) and, among those, very few plan on sitting out.
In February, ONC recognized six organizations that have been accepted for onboarding as Qualified Health Information NetworksTM (QHINsTM) under TEFCA. These six candidate QHINs have committed to achieving “go-live” by the end of 2023. With that date just around the corner, we thought the time was right to better understand awareness and plans to participate in TEFCA among the broader health care delivery system. A seventh candidate QHIN was accepted for onboarding in May.
In the 2022 AHA Information Technology Supplement survey, fielded through December 2022, almost 2,500 leaders of non-federal acute care hospitals reported on their awareness of TEFCA and their plans to participate. Even with TEFCA having been out since January 2022, but go-live still several months away, we wanted to identify whether health care providers were aware of TEFCA, whether those aware of TEFCA plan to participate, and whether some types of hospitals were less likely to know about TEFCA and thus, less likely to plan to participate.
Figure 1: Hospital Awareness of and Plans to Participate in TEFCA
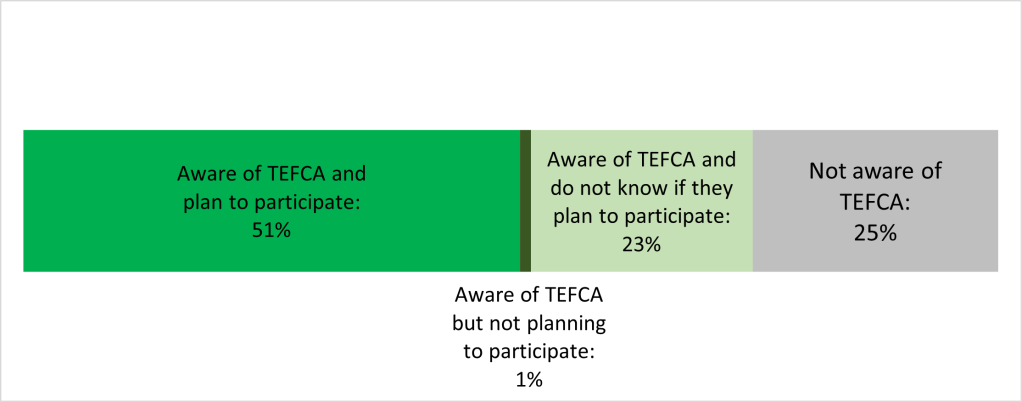
Our analysis of the survey data shows that half (51%) of hospitals are aware of TEFCA and plan to participate (Figure 1). More impressive, only 1% of responding hospitals said that they were aware of TEFCA and were NOT planning to participate. We think that reflects widespread enthusiasm for TEFCA with few concerns preventing participation among those knowledgeable enough to have developed plans.
The other key takeaway is that 48% of hospitals have not yet decided whether they will participate in TEFCA when responding to the survey. We suspect that the recent announcement of the first group of QHINs approved for onboarding reduced the percentage of hospitals that are not aware of TEFCA today compared to the survey period. Nevertheless, the fact that a significant percentage of hospitals either didn’t know about TEFCA or didn’t know their plans as recently as December points to the value of ongoing outreach and education work for ONC, the Recognized Coordinating Entity® (RCETM) that implements and maintains the Common Agreement, and other organizations that want to see TEFCA flourish. That work is especially important because it seems that knowledge is the key barrier: once hospital leaders know about the potential benefits of TEFCA, they want to participate.
Beyond these overall numbers, we looked at differences in awareness and plans to participate in TEFCA by a handful of key tracer hospital characteristics (Figure 2). Across characteristics, there was a key signal that less resourced hospitals were both less likely to be aware of TEFCA and less likely to plan to participate when they were aware:
- Just 29% of independent hospitals plan to participate in TEFCA compared to 61% of multi-hospital system members;
- 32% of critical access hospitals plan to participate compared to 59% of non-critical access hospitals; and
- Just 18% of hospitals that do not participate in one of three national networks (eHealth Exchange, CommonWell or Carequality) plan to participate compared to 65% of hospitals that already participate in one of the national networks.
Figure 2: Hospital Awareness of and Plans to Participate in TEFCA, by Key Hospital Characteristics
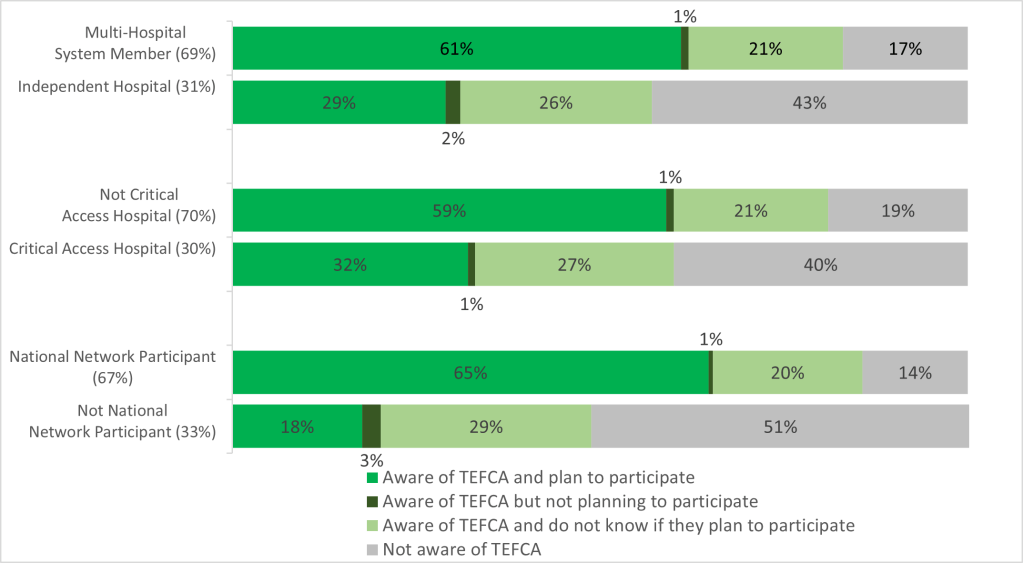
Acknowledging that we are in the early stages of supporting data exchange through TEFCA, these trends, whereby low-resource hospitals are less likely to plan to join TEFCA, give us insight into opportunities for more education and engagement with these hospitals. The trend we see here is not surprising but rather reflects broader trends in data ONC has recently published on hospitals, physicians, and individuals, as well as broader work on the “digital divide” in the use of health IT. A key goal of TEFCA is to shrink this digital divide by shining a light on these gaps, lowering the cost and complexity of interoperability, and identifying resources to support broader access to nationwide interoperability networks.
We will continue to develop educational resources that are designed to inform interested parties about how TEFCA will work and how it may cut down on their costs. For instance, the RCE recently published the Informational Resource for Flowing Down Common Agreement Provisions into Framework Agreements, which is intended to assist QHINs, Participants, and Sub-participants in complying with their Common Agreement flow-down obligations. This resource, along with others the RCE has published, will save entities interested in joining TEFCA significant time, resources, and legal fees.
In addition, we expect that QHINs, once officially designated, will engage in significant outreach activities, which will also be a means of disseminating information to providers that are currently not aware of TEFCA.
Finally, we are working with our federal and state partners to identify opportunities for outreach and resources tailored to the needs of underserved providers.
ONC, the RCE, and our partners are committed to enabling TEFCA adoption to improve care and care coordination, reduce administrative overhead, expand public health reporting, facilitate emergency preparedness and response, and increase patient access to their health care information.






