
An official website of the United States government
Here’s how you know
Official websites use .gov
A
.gov
website belongs to an official government organization in the
United States.
Secure .gov websites use HTTPS
A
lock
(
) or
https://
means you’ve safely connected to the .gov website. Share sensitive
information only on official, secure websites.
Electronic Prescribing of Controlled Substances (EPCS) among Office-Based Physicians, 2017
No. 49 | September 2019
In October 2018, Congress passed the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act to address the opioids epidemic (1). This legislation mandated that all Medicare Part D providers electronically prescribe controlled substances (EPCS) by 2021. EPCS is beneficial because it can help providers integrate prescription drug information into electronic health records (EHRs) more directly, which can improve patient safety and reduce diversion and fraud. This brief uses data from the 2017 National Electronic Health Records Survey, a nationally representative survey of office-based physicians, to understand rates of EPCS. It explores variation by physician characteristics; including adoption of certified EHRs, physician specialty, practice size and ownership, rural or urban practice, participation in value based payment models, and interoperability with other physicians.
Highlights
- In 2017, 32 percent of office-based physicians that prescribed controlled substances did so electronically.
- Approximately one third of physicians with computerized systems for prescribing prescriptions, electronically prescribe controlled substances.
- Larger physician practices and practices owned by hospitals had the highest rates of physician EPCS.
- Physicians that engaged in the four domains of interoperability were more likely to EPCS than physicians that did not engage in the four domains.
- Physicians participating in CMS Innovation Models had significantly higher rates of EPCS compared to physicians that did not participate in these programs.
In 2017, 32 percent of office-based physicians that prescribed controlled substances did so electronically.
Figure 1: Percent of office based physicians that prescribed controlled substances and did so electronically, 2017.
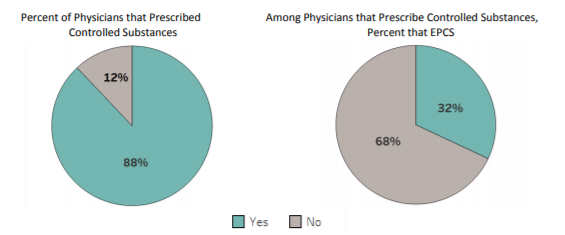
Note: The sample consists of 2,362 office based physicians.
- In 2017, 88 percent of physicians prescribed controlled substances.
Approximately one third of physicians with computerized systems for prescribing prescriptions, electronically prescribe controlled substances.
Table 1: Percent of office based physicians that have a certified EHR^ and EPCS by capability of computerized systems, 2017.
| % Physician with Electronic Prescribing Capabilities | Among Physicians with the Electronic Capability | ||
|---|---|---|---|
| % Physicians with a Certified EHR | % Physicians that EPCS | ||
| Does the reporting location use a computerized system to order prescriptions? | |||
| No (reference) | 14 | – | – |
| Yes | 86* | 89 | 36 |
| Among physicians with computerized orders for prescriptions, are prescriptions sent electronically to the pharmacy? | |||
| No (reference) | 16 | – | – |
| Yes | 84* | 89 | 36 |
| Among physicians with computerized orders for prescriptions, are warnings of drug interactions or contraindications provided? | |||
| No (reference) | 17 | – | – |
| Yes | 83* | 89 | 37 |
| Does the reporting location use a computerized system to reconcile lists of patient medications to identify the most accurate list? | |||
| No (reference) | 11 | – | – |
| Yes | 89* | 88 | 35 |
| Physicians with all four capabilities above | |||
| No (reference) | 23 | – | – |
| Yes | 77* | 90 | 38 |
Note: The sample consists of 2,125 office based physicians who prescribed opioids. *Significantly higher than the reference category (p<0.05). ^See Definitions
- Eighty six percent of physicians have computerized systems for ordering prescriptions. Among these physicians, 89 percent have a certified EHR and 36 percent EPCS.
- Among physicians with computerized systems to order prescriptions, 84 percent of physicians also have the capability to electronically send prescriptions to the pharmacy and 83 percent of physicians’ systems can provide warnings of drug interactions or contraindications.
- Rates of using certified EHRs and EPCS are consistent across the different electronic capability categories, approximately 89 percent of physicians have certified EHRs and 35-40 percent of physicians EPCS regardless of which electronic capabilities they have.
- Seventy-seven percent of physicians have all four capabilities, but rates of certified EHRs and EPCS do not increase; approximately 90 percent of physicians had certified EHRs and 38 percent EPCS.
Physician practices that were larger or owned by hospitals had the highest rates of electronically prescribing controlled substances.
Table 2: Percent of office based physicians that EPCS by physician characteristics, 2017.
| % Physicians that EPCS | |
|---|---|
| Practice Size | |
| 1 Physician (reference) | 23 |
| 2-3 Physicians | 23 |
| 4-10 Physicians | 35* |
| 11-100 Physicians | 37* |
| More than 100 Physicians | 59* |
| Practice Ownership | |
| Physician / Physician Group (reference) | 25 |
| Insurance company, health plan, HMO or other health care corporation | 41* |
| Community Health Center | 26 |
| Hospital | 44* |
| Geographic Location | |
| Rural (reference) | 25 |
| Urban | 32 |
| Physician Specialty | |
| Primary Care (reference) | 32 |
| Surgical Specialty | 31 |
| Medical Specialty | 31 |
Note: The sample consists of 2,125 office based physicians who prescribed opioids. *Significantly higher than the reference category (p<0.05).
- Physicians in practices with four or more physicians were significantly more likely to EPCS compared to physicians in smaller practices.
- Rates of EPCS were significantly higher among physicians in practices owned by hospitals (44 percent) or insurance companies/ health plans/ Health Maintenance Organizations (HMOs) (41 percent) compared with physician owned practices (25 percent).
- There was no significant difference in rates of EPCS between physicians in rural and urban areas
- There was no difference in rates of EPCS by physician specialty; approximately one third of physicians electronically prescribed controlled substances across all specialties.
Physicians that engaged in the four domains of interoperability were more likely to EPCS than physicians that did not engage in the four domains.
Figure 2: Percent of office based physicians that EPCS by ability to electronically send, receive, find, and integrate patient health information, 2017.
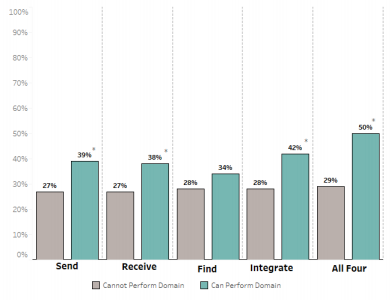
Note: See “Definitions” for full description of the four domains of interoperability. The sample consists of 2,125 office based physicians who prescribed opioids. Physicians that reported “don’t know” or “missing” for each of the domains were categorized as not being able to engage in the domain. Among physicians that prescribe controlled substances, 36 percent of physicians can send patient health information, 39 percent can receive patient health information, 55 percent can find patient health information, 28 percent can integrate patient health information, and 11 percent can send, find, receive, and integrate patient health information. *Significantly higher than physicians that did not engage in that domain of interoperability (p<0.05).
- Thirty-nine percent of prescribers that can send patient health data electronically EPCS compared to 27 percent of physicians that cannot send patient health data electronically.
- There was no difference in rates of EPCS between physicians that could and could not find patient health information.
- Physicians without the ability to send or receive patient health information from physicians outside their organization had the lowest use of EPCS, 27 percent.
- Physicians that engaged in all four interoperability domains had the highest rates of EPCS, 50 percent.
Physicians participating in CMS Innovation Models had significantly higher rates of EPCS compared to physicians that did not participate in these programs
Figure 3: Percent of office based physicians that EPCS by participation in Centers for Medicare and Medicaid (CMS) Innovation Models, 2017.
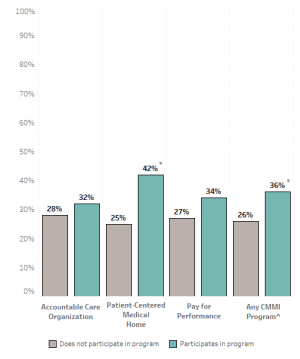
Note: The sample consists of 2,125 office based physicians who prescribed opioids. Among physicians that prescribe controlled substances, 51 percent participated in the Accountable Care Organization program, 38 percent participated in the Patient Centered Medical Home Program, 49 percent participated in the Pay for Performance program, and 57 percent participated in any CMMI program. ^”CMMI” is an abbreviation for the Centers for Medicare and Medicaid Services’ (CMS) Center for Medicare and Medicaid Innovation (CMMI). *Significantly higher than physicians that did not participate in the program (p<0.05).
- Participants of the Patient Centered Medical Home Program had the highest rates of EPCS; 42 percent of physicians participating in this program electronically prescribed controlled substances.
- Physicians that participated in any CMMI program had higher rates of EPCS, 36 percent, compared to physicians that did not participate in any program, 26 percent.
- Physicians that did not participate in the Patient Centered Medical Home Program had the lowest rates of EPCS, 25 percent.
Summary
Electronic prescribing of controlled substances (EPCS) can streamline provider workflow, improve medication safety, and enable more efficient pain management for patients. Prior research has shown that nearly 90 percent of all non controlled substances are prescribed electronically, but that electronic prescribing rates for controlled substances are low (2) (3). This analysis finds that in 2017, 32 percent of office based physicians that prescribed controlled substances did so electronically.
There is a relationship between the technology physicians possess and whether a physician also prescribes controlled substances electronically. Most physicians (86 percent) have a computerized system to order prescriptions; which is comparable with the national rate of physicians with an EHR (86 percent) (5). Approximately 90 percent of physicians with electronic prescription capabilities use certified EHRs. Moreover, approximately 36 percent of physicians with electronic systems to order prescriptions, also EPCS. This rate is similar to rates of EPCS among physicians with additional electronic capabilities of the computerized systems.
Physician characteristics are also an important factor for EPCS. Larger physician practices had significantly higher rates of EPCS. In 2017, 59 percent of physicians in practices of 100 or more physicians EPCS compared to only 23 percent of physicians in practices of 3 or fewer physicians. Similarly, more than 40 percent of physicians in practices owned by a hospital or insurance company EPCS compared to 25 percent of physicians in practices owned by physicians or community health centers. There were no statistical differences between physicians based in urban or rural areas or by physician specialty.
The relationship between interoperability and EPCS was mixed. Physicians with the ability to send, receive, or integrate patient health information from outside a physicians’ organization were significantly more likely to EPCS. However, this relationship did not hold for physicians that could find patient health information from outside their organization. For physicians that engaged in all four interoperability domains, 50 percent of them electronically prescribed controlled substances, compared to 29 percent of physicians who were not engaged in all four domains, a significant difference.
Finally, physicians that participated in CMS’ Innovation Models programs had higher rates of EPCS, 36 percent, compared to physicians that did not participate in these programs, 26 percent. Participating in the Patient Centered Medical Home Program was associated with the highest rates of EPCS, 42 percent.
Taken together, physicians with more electronic capabilities, those owned by hospitals or part of integrated health systems, and those that participate in CMMI programs, are more likely to EPCS. Through implementation of the SUPPORT for Patients and Communities Act, CMS will require controlled substances covered under Medicare Part D to be electronically prescribed. The data presented in this brief can be used as a baseline to help inform the implementation and evaluation of the SUPPORT Act as well as other related policies.
Definitions
Send patient health information: The use of an EHR or web portal to send patient health information to other providers outside their medical organization
Receive patient health information: The use of an EHR or web portal to receive patient health information from other providers outside their medical organization.
Find or Query patient health information: Physicians electronically search for patient health information from sources outside of their medical organization.
Integrate patient health information: Use of an EHR to integrate summary of care records or other types of patient health information without special effort like manual entry or scanning into an EHR.
Certified EHR: Physicians indicated that their reporting location used an EHR, and that the EHR met the criteria for Meaningful Use.
Data Source and Methods
The Centers for Disease Control and Prevention’s National Center for Health Statistics conducts the National Electronic Health Records Survey (NEHRS) survey on an annual basis. Physicians included in this survey provide direct patient care in office-based practices and community health centers; excluded are those who do not provide direct patient care (radiologists, anesthesiologists, and pathologists). Additional documentation regarding the survey is here: https://www.cdc.gov/nchs/nehrs/index.html
References
1. Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act, Section 2003. https://www.congress.gov/bill/115th-congress/house-bill/6/text
2. Gabriel M.H., Swain M. (July 2014). E-Prescribing Trends in the United States, no.18. Office of the National Coordinator for Health Information Technology: Washington DC.
3. Johnson C., Barker W., Pylypchuk Y. & Parasrampuria S. (April 2019). Electronic Prescribing of Controlled Substances among Medicare Part D Prescribers 2015-2016, no. 44. Office of the National Coordinator for Health Information Technology: Washington DC.
4. Patel V., Pylypchuk Y., Parasrampuria S. & Kachay L. (May 2019). Interoperability among Office-Based Physicians in 2015 and 2017. ONC Data Brief, no. 47. Office of the National Coordinator for Health Information Technology: Washington D.C.
5. Ogburn D.F., Myrick K.L. (April 2019). Table 1. Percentage of Office-based Physicians with Selected Geographic Characteristics, by Use of any Electronic Health Record (EHR)/ Electronic Medical Record (EMR) and Those that Use a Certified EHR/EMR system: National Electronic Health Records Survey, 2017. National Center for Health Statistics.
Acknowledgements
The authors are with the Office of Technology, within the Office of the National Coordinator for Health Information Technology. The data brief was drafted under the direction of Mera Choi, Director of the Technical Strategy and Analysis Division and Talisha Searcy, Branch Chief of the Data Analysis Branch.
Suggested Citation
Parasrampuria S., Blanco M., & Barker W. (September 2019) Electronic Prescribing of Controlled Substances among Office-Based Physicians, 2017, no.49. Office of the National Coordinator for Health Information Technology: Washington DC.
